MIPS 2020 Final Rule in Easy-to-Read Bullets
The Centers for Medicare & Medicaid Services (CMS) published the Calendar Year (CY) 2020 FINAL Rule for the Medicare Physician Fee Schedule (MPFS). The MPFS dictates Medicare rates and policies under Part B, while the Quality Payment Program (QPP) implements two key value-based payment programs: the Merit-Based Incentive Payment System (MIPS) and Alternative Payment Models (APMs). The proposal is very long at over 1700 pages!
As experts of the MIPS Quality Payment Program, we are bringing you the MIPS highlights to you section-by-section segments and give you the most pertinent bullets.
Overview
The threshold to avoid a penalty is changing. The performance threshold is rising from 30 points to 45!
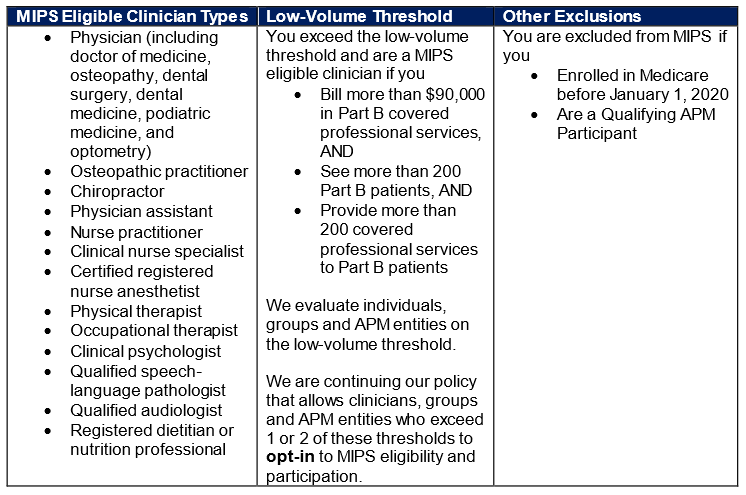
Eligibility requirements remain unchanged.
The category weights will remain the same as they were in 2019 but will change in future years!
MIPS Value-based Pathways (MVP) will be implemented gradually for the beginning of the 2021 performance period.
Under the MVP, the clinician quality program will move away from reporting on activities and measures from the four performance categories (Quality, Cost, Improvement Activities and Promoting Interoperability) to a unified set of measures and activities centered on a specific condition or specialty.
CMS created some illustrative diagrams regarding the MIPS Value Pathways: MIPS Value Pathways Diagram
Quality
Category weight remains at 45%
Data completeness increases to 70%
SEVERAL MEASURE CHANGES!
The details behind each measure are included in the Final Rule Appendices. Here is a very HIGH-LEVEL summary of the changes to Quality measures for the 2020 performance year.
NEW Measures
476, 477, N/A Adult Immunization Status, 478
REMOVED Measures
HINT: If you are reporting any of these measures in 2019, they will need a replacement measure for 2020.
68, 91, 109, 131, 160, 165, 166, 179, 192, 223, 255, 262, 271, 325, 328, 329, 330, 343, 345, 346, 347, 352, 353, 361, 362, 371, 372, 388, 411, 417, 428, 442, 446, 449, 454, 456, 467, 474
SUBSTANTIVE CHANGES to Measures
If you are reporting any of these measures in 2020, review the spec sheet b/c there has been a significant change to the specifications
1, 5, 7, 8, 9, 19, 66, 76, 102, 107, 110, 111, 112, 113, 117, 119, 128, 134, 143, 144, 176, 177, 178, 180, 181, 182, 191, 217, 218, 219, 220, 221, 222, 226, 236, 238, 240, 243, 268, 282, 286, 290, 305, 317, 326, 332, 335, 336, 337, 342, 348, 370, 377, 378, 379, 382, 385, 391, 392, 393, 394, 405, 415, 416, 418, 438, 439, 440, 441, 448, 450, 459, 460, 461, 462, 469, 470, 471, 472, 473, 475, 282, 288
Promoting Interoperability
Requires 2015 CEHRT
90 Day Reporting Period continues
Qualifying exemptions in this category will still re-weight the 25 points to Quality
Still performance based scoring. (Not all-or-nothing.)
Security Risk Analysis still a scoreless pre-requisite
CMS finalized their proposal to remove the opioid treatment agreement measure.
CMS is keeping the Query of Prescription Drug Monitoring Program (PDMP) measure as optional. Reporting will be a “Yes” or “No” instead of a numerator and denominator.
Improvement Activities
More than 100 activities to choose from
Activity Edits Include:
Add 2 improvement activities
Modify 7 improvement activities
Remove 15 improvement activities
Double-check the activities you plan to use!
Most important, CMS is increasing the participation threshold for group reporting from a single clinician to 50% of the clinicians in the practice!
This means to use an IA for a group 50% or more of the clinicians must do the activity for at least a continuous 90 days!
Cost
Staying at 15%
Changes to two of the measure types the Medicare Spending Per Beneficiary Clinician measure and Total Per Capita Cost measure.
Assign responsibility for services to a larger number of clinicians
Improve risk adjustment timeline
Avoid assigning costs that are incurred before a clinician begins providing services to a patient
Additionally, CMS proposes increasing the number of episode-based measures from 8 to 18 by adding 10 new measures:
NEW
Acute Kidney Injury Requiring New Inpatient Dialysis
Elective Primary Hip Arthroplasty
Femoral or Inguinal Hernia Repair
Hemodialysis Access Creation
Inpatient Chronic Obstructive Pulmonary Disease (COPD) Exacerbation
Lower Gastrointestinal Hemorrhage
Lumbar Spine Fusion for Degenerative Disease, 1-3 Levels
Lumpectomy Partial Mastectomy, Simple Mastectomy
Non-Emergent Coronary Artery Bypass Graft (CABG)
Renal or Ureteral Stone Surgical Treatment
EXISTING
Elective Outpatient Percutaneous Coronary Intervention (PCI)
Knee Arthroplasty
Revascularization for Lower Extremity Chronic Critical Limb Ischemia
Routine Cataract Removal with Intraocular Lens (IOL) Implantation
Screening/Surveillance Colonoscopy
Intracranial Hemorrhage or Cerebral Infarction
Simple Pneumonia with Hospitalization
ST-Elevation Myocardial Infarction (STEMI) with Percutaneous Coronary Intervention (PCI)
Overall
MIPS eligible clinicians and groups should become familiar with the changes for the 2020 reporting year. The QPP Final Rule has established higher performance thresholds and payment adjustments, so more reporting and planning will be necessary to avoid any penalties.
Additional Resources
If you would like to read all -2400+ pages of the FINAL RULE you can find it here.
All of the QPP web resources will be updated on or before January 1, 2020.