Why Small Practices Should NOT Skip Promoting Interoperability
The Merit-based Incentive Payment System (MIPS) is a critical program that affects healthcare practices of all sizes. While it might seem advantageous for small practices to avoid certain categories due to the MIPS automatic reweighting, doing so could be a missed opportunity. Let's break down why.
Understanding MIPS Scoring
The MIPS program is divided into four categories, with a total possible score of 100 points. For small practices with 15 or fewer eligible clinicians, there's an automatic reweighting. Here's how the scoring breaks down based on CMS's default rules:
Small Practices (15 or fewer clinicians)
Quality: 40%
Improvement Activities (IA): 30%
Cost: 30%
Larger Practices (16 or more clinicians) and Small Practice that Report PI
Quality: 30%
Improvement Activities (IA): 15%
Cost: 30%
Promoting Interoperability: 25%
This reweighting, when shifting from a large to a small group, increases the significance of Quality by 10% and doubles the weight of Improvement Activities to 30%.
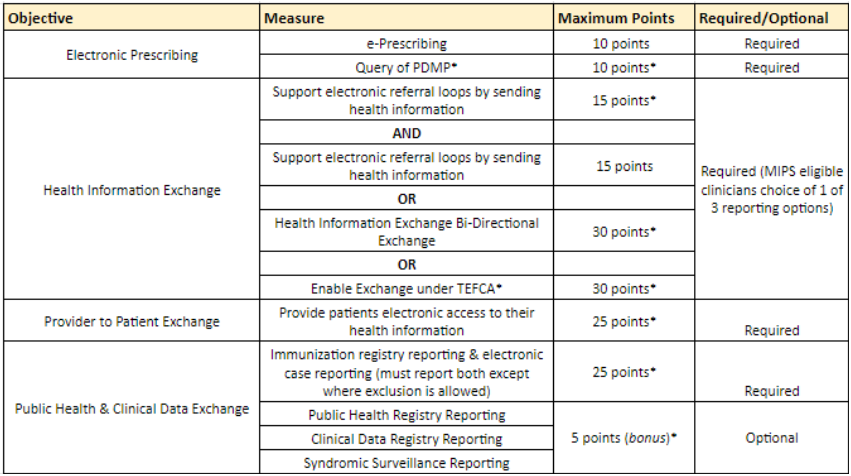
What’s Included in PI for 2023
Below is the breakdown of 2023 measures. Many of these persist from years past and may be things your clinicians or practice are already doing, such as ePrescribing. Even things like health information exchange are not as daunting as they might seem. The 2023 requirement may easily be met if your EHR vendor is supporting a partnership to exchange information under TEFCA or if your practice participates with say its state health information exchange (HIE) network. The PI category is a minimum 90 consecutive days performance period. It’s also important to note that the category remains performance based with several potential exclusions, if a practice qualifies.
Why Skipping a Category Might Not Be Wise
It may seem, at first glance, that fewer categories to address could be an advantage, especially since the "Improvement Activities" category (which is often perceived as one of the easiest) benefits small practices more.
However, with the challenges around Quality measure benchmarks, performance decile ranges, and the possibility of measures being topped out, earning the full 60 achievement points in Quality is quite a challenge. This makes it tough for most practices to maximize the full 40% value in the Quality category. Simply put: the Quality measure available through your EHR or registry systems may be limited by their benchmarks and relative decile potential. For example, if you report Measure 128, Preventive Care for BMI screening and follow-up as a CQM the maximum number of points is 7 unless you have an absolute perfect score. The same is true for the Dementia function status assessment, measure 282, where a maximum of 3 points exists. Regardless of the tools you use it can be incredibly difficult to maximize your Quality score even with excellent overall performance.
A Real-Life Example
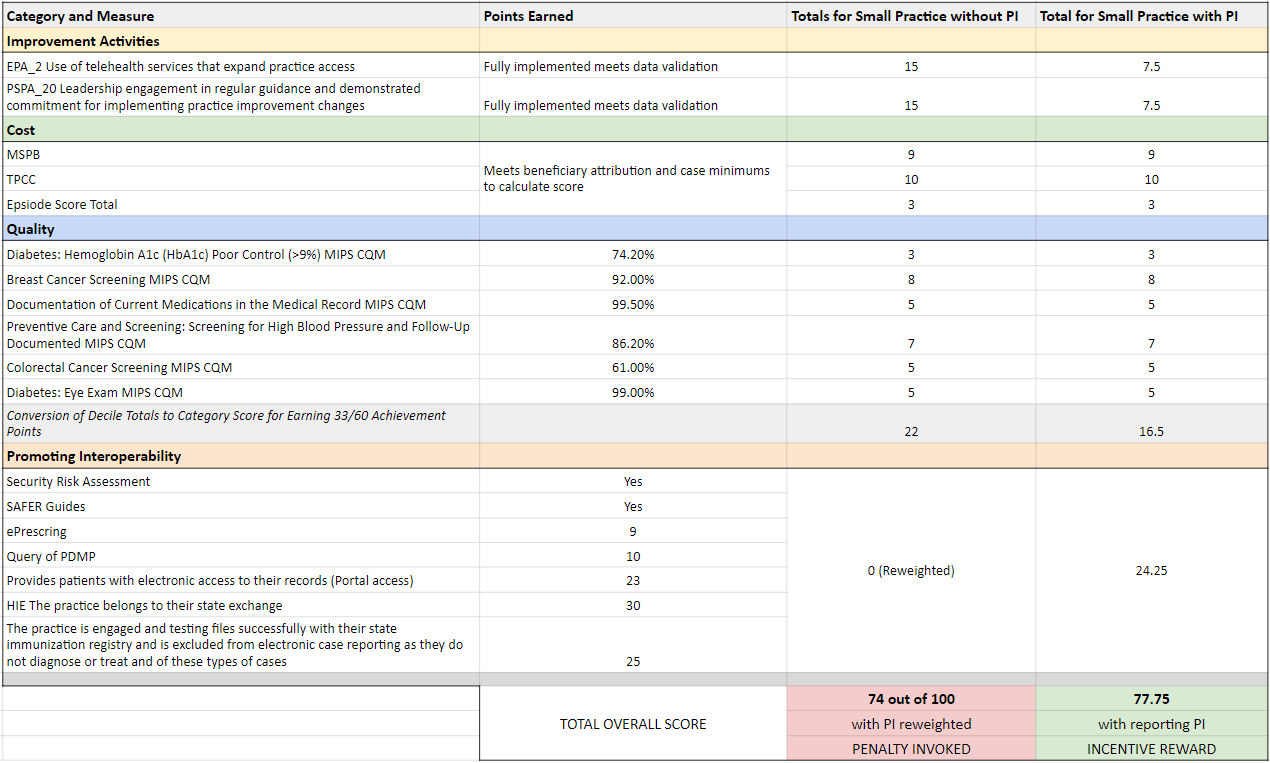
To better understand, let's examine an example using common measures from 2023.
Let’s assume a few things:
The group will report the right number and weight of Improvement Activities to earn their full points.
Their total Cost score will be assessed but they only earn 22/30 points overall.
Their Quality measures include a compilation of types and are mostly primary care related in nature. There are no year-over-year improvement points.
Where we demonstrate PI reporting, the group is using certified EHR technology and has relatively good but not perfect scores.
Lastly, the practice will not earn any complex patient bonus points.
Here’s the breakdown of what it would look like were the practice to choose to proceed without reporting PI, and what it looks like when they elect to report instead of the automatic reweighting:
You can see that with a combination of Quality measure and relatively good performance reporting PI can be the difference between penalty and an incentive since the score threshold in 2023 is 75 out of 100 overall points.
The Lesson: Consider PI
While the MIPS program offers some leeway for small practices, it's essential to understand the nuances and potential consequences of skipping certain categories. The majority of small practices we assist choose to report on Promoting Interoperability, not just to tick a box, but to genuinely increase their score and incentive potential. Before making a decision, it's critical to evaluate all aspects of the MIPS program and choose a strategy that ensures optimal outcomes for your practice. Our team helps our clients on a monthly basis review these critical “what if” scenarios to identify the best possible ways to maximize their score through all available avenues.
If you need help with the Promoting Interoperability category or have other MIPS questions give us a call. We know your time is valuable and our team are MIPS experts who can help you save time and frustration while helping ensure your MIPS score provides an ROI.
hello@chirpybirdinc.com Phone: 888-647-7247